What Is Cognitive Behavioral Therapy for Insomnia?
The Psychological Approach to Getting Better Sleep
Unfortunately, insomnia is far from uncommon. For an estimated 70 million adults in America, it’s a problem that literally keeps them up at night.
According to the American Academy of Sleep Medicine (AASM), 30 to 35 percent of adults experience brief insomnia symptoms, 15 to 20 percent have a short-term insomnia disorder, and 10 percent have a chronic insomnia disorder.
A single sleepless night can have self-evident side effects. The next day, you may feel groggy or have trouble concentrating at work. While a few exhausting days like this may not be a big deal, prolonged sleep deprivation and chronic insomnia can have severe implications for your overall health.
Common Ways to Treat Insomnia
In the short term, sleep deprivation can cause irritability, excessive daytime sleepiness, and impaired judgment, sometimes leading to accidents, injuries, and work-related errors.
Meanwhile, the long-term risks of insomnia develop gradually and can be harder to detect. Chronic problems with sleep can contribute to weight gain, symptoms of depression and anxiety, hypertension and other cardiovascular complications, weakened immunity, and diabetes.
Sleep is as essential to human biology as food, water, and oxygen. But it’s about more than just survival—getting quality sleep directly enhances your quality of life. To take back control of their lives, many people have turned to prescription drugs, natural sleep aids, and other home remedies for insomnia treatment.
Unfortunately, many sleep medications cause significant side effects, have diminishing returns, and can lead to dependency. While effective, prescription drugs for sleep aren’t always a viable long-term solution.
On the other hand, many people with trouble sleeping do find relief through sleep aids and natural remedies such as over-the-counter antihistamines, melatonin supplements, and CBD. However, antihistamines aren’t suitable for long-term insomnia treatment, and many natural sleep aids currently lack regulation or confidence from the scientific community. Also, sleep aids tend to treat insomnia symptoms, not address the underlying issues.
So, what treatment options does that leave?
It’s a lot easier said than done, but making behavioral changes can transform your sleep health. By modifying your diet, exercise regimen, nighttime routines, and other lifestyle habits, you can improve your sleep without any medications or supplements.
Many sleep specialists and other medical professionals now point to cognitive behavioral therapy for insomnia (CBT–I or CBTi) as the safest—and most effective—way to treat insomnia. CBT-I programs take a holistic approach to sleep health and can incorporate diet, exercise, sleep schedules, and more.
CBT-I programs take a holistic approach to sleep health and can incorporate diet, exercise, sleep schedules, and more.
What Is Cognitive Behavioral Therapy?
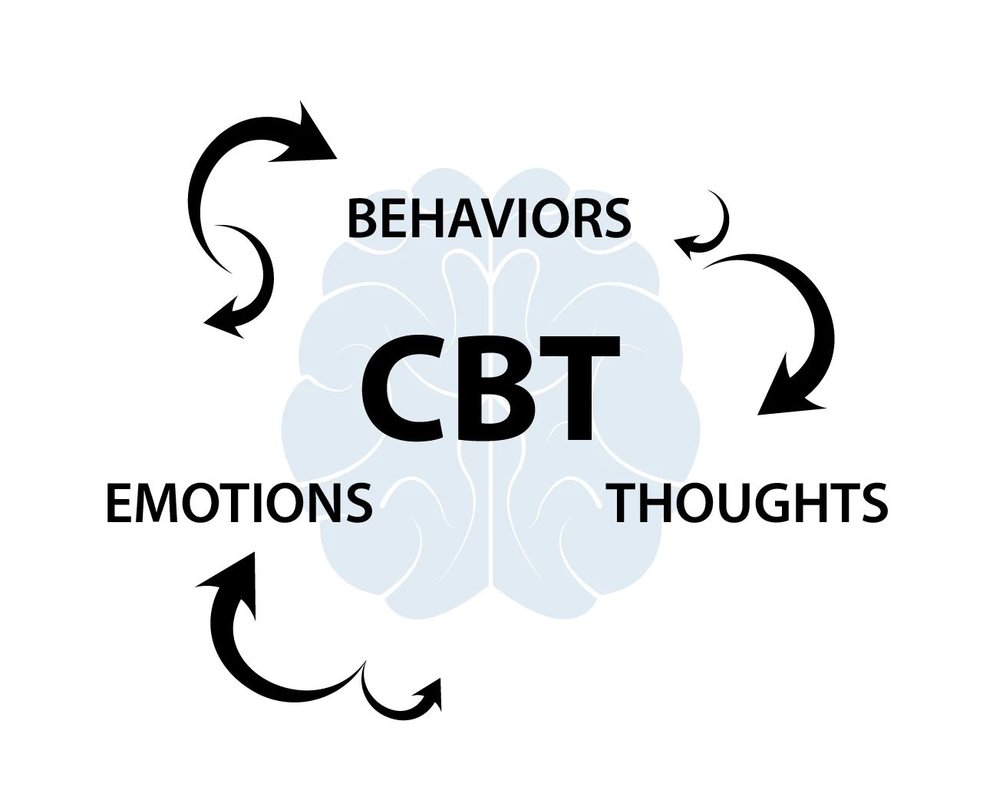
Before delving into the merits of CBT-I, you may want a clearer picture of general cognitive behavioral therapy (CBT).
This approach to treating mental disorders originated in the 1960s when psychiatrist Dr. Aaron T. Beck developed a technique he then called “cognitive therapy.” In his cognitive model, Beck theorized that the way people react to situations, behaviorally and emotionally, is more connected to their perception of the situation than the situation itself.
Beck’s proposed treatment—now widely accepted and known as “cognitive behavioral therapy”—addresses the patient’s perception of events and the world around them. CBT focuses on the “automatic thoughts” that different situations evoke, which are often distorted by distress. The therapy helps patients identify and evaluate these reactionary thoughts and change their thinking to better reflect reality.
Put simply, CBT helps people understand their way of thinking and teaches them the skills they need to modify negative thought patterns. Today, therapists use CBT to treat depression, anxiety disorders, eating disorders, substance abuse, and more—including insomnia.
How Does CBT Work for Sleep?
Instead of targeting the symptoms of insomnia, CBT-I focuses on the behaviors, thoughts, and beliefs that inhibit sleep. This structured program first helps patients identify the lifestyle habits and thought patterns that make it difficult to get quality sleep, then helps them to eliminate or replace these behaviors with positive practices.
Everyone responds to treatment differently, but many people see improvement in their sleep after two to six therapy sessions. Depending on what you struggle with and what you’ve tried in the past, your therapist may introduce a few of the following techniques.
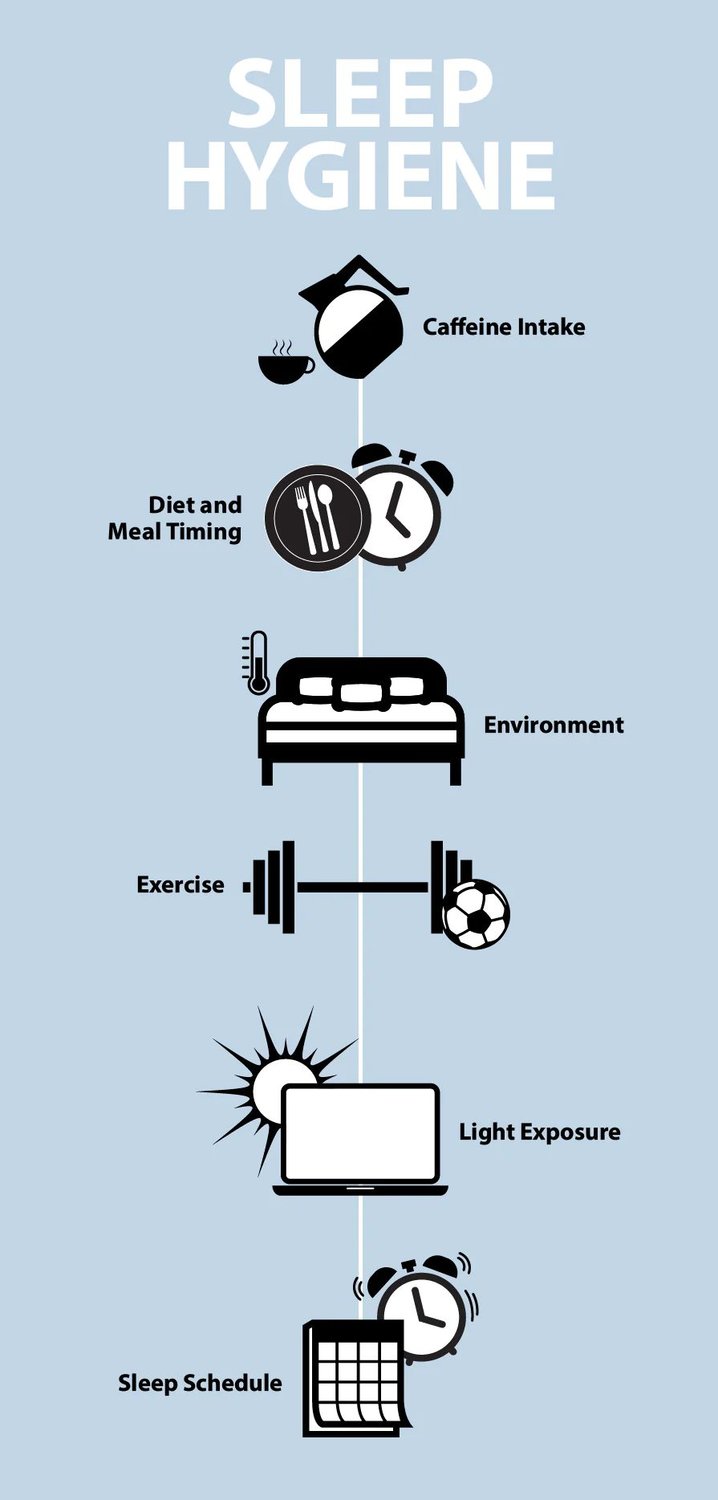
Sleep Hygiene Education
First and foremost, CBT-I provides patients with psychoeducation about sleep, specifically sleep hygiene. Your therapist will help you understand the mechanisms of sleep, such as circadian rhythms, and explain best practices for consistent, quality sleep. Sleep hygiene encompasses topics like:
- Caffeine consumption
- Maintaining a sleep schedule
- Morning and bedtime routines
- How light exposure affects your circadian rhythm
- How diet and exercise impact sleep
Stimulus Control
This cognitive behavioral therapy technique focuses on the conditions that promote or prevent the mind and body from preparing for sleep. As explained by Stanford Health Care, stimulus control therapy is “designed to strengthen the bed as a cue for sleep and weaken it as a cue for wakefulness.”
During this phase of treatment, CBT-I practitioners give patients instructions to follow that help reinforce these cues, such as:
- Waking up (and getting out of bed) at the same time every day
- Going to bed only when you feel tired
- Getting out of bed if you can’t fall asleep, and only return when you feel tired
- Avoiding excessive napping
Sleep Restriction or Compression
If it sounds counterintuitive to restrict sleep to combat insomnia, don’t worry—this CBT-I technique aims to reduce the total time spent in bed, not the amount of actual sleep you get each night. Though it may cost you some shut-eye at the beginning, the treatment will gradually get you back on a regular sleep schedule built around quality rest.
At the beginning of sleep restriction treatment, patients are instructed to only spend as much time physically in bed as they usually sleep each night. So, if you typically spend a couple of hours trying to drift off but ultimately only sleep for six hours, you’ll start your sleep restriction treatment by limiting your total time spent in bed to six hours.
If effective, this training will reduce the amount of time you spend awake while laying in bed—but you’ll still feel sleep-deprived. However, once your body adjusts to this restricted time frame, your CBT-I therapist will gradually extend the time you’re allowed to spend in bed in 15 to 30-minute increments over the course of a few weeks.
With each increment, you should spend more time asleep; extending the time you spend in bed should not add to the time you spend trying to fall asleep. According to Stanford Health Care, this process ultimately helps you achieve optimal sleep efficiency.
Relaxation Training, Paradoxical Intention, and Reducing Sleep-Interfering Arousal
Though different in practice, these three CBT-I techniques all share a common goal: they all help you calm the body and mind, allowing sleep to take over naturally.
Relaxation training is exactly what it sounds like. Your therapist or practitioner will teach you calming techniques such as muscle relaxation, imagery, and mediation.
Paradoxical intention training encourages patients to take their minds off falling asleep. If you harp on how much you need rest or how long it’s taking you to fall asleep, the pressure you put on yourself paradoxically prevents you from drifting off. Staying “passively awake” means you try your best to avoid any thoughts about falling asleep that add unnecessary stress and work against your efforts.
Similar to paradoxical intention, the sleep-interfering arousal reduction technique helps people fall asleep naturally, not by willpower. This practice focuses on stress management skills, relaxation, and reducing worry related to sleep. Reducing sleep-interfering arousal tactics can include calming activities before bed, moving clocks out of sight, and creating a comfortable environment.
Is There Evidence That CBT-I Works?
Now that you understand the theory and logistics of cognitive behavioral therapy for insomnia, you may still have a lingering question: does it really work?
As previously mentioned, many medical professionals and sleep experts favor CBT-I over other insomnia treatments and recommend patients try it before turning to medications or supplements. But does data support the efficacy of CBT-I?
In February of 2021, the AASM published its latest clinical practice guidelines and officially recommended CBT for adults with chronic insomnia. Before making this recommendation, the AASM commissioned a task force to perform a systematic review of published studies dealing with behavioral and psychological treatments for insomnia.
The task force analyzed the results of 49 studies measuring both sleep quality and sleep latency outcomes. According to the AASM’s meta-analysis, CBT-I demonstrates “significant mean improvement” in both areas for subjects with insomnia.
Free Resources for Exploring CBT for Insomnia
Interested in giving CBT-I a try? Fortunately, you can explore CBT-I and implement some of the techniques described above without paying out of pocket for one-on-one sessions with a specialist.
While in-person, individualized therapy with a professional is still strongly recommended, you can still experience the benefits of CBT-I through other means or use free tools to assist you on your journey.
For example, the U.S. Department of Veterans Affairs (VA) offers a free Insomnia App that employs the principles of CBT-I. The app caters to everyone, not just veterans or those with PTSD. You can also watch a free CBT-I training video on the VA.
The Anxiety & Depression Association of America website also offers an educational webinar on CBT-I presented by Dr. Virginia Runko, a licensed clinical psychologist board-certified in behavioral sleep medicine.
Just remember, these services don’t replace therapy, and you should always consult your doctor before starting any health or mental-health-related programs.
Conclusion
CBT-I can entail a lot of hard work and dedication, and it isn’t as easily accessible as over-the-counter sleep aids and supplements. However, it is an all-natural approach and highly recommended by the AASM and many health professionals.
Unlike many other insomnia treatments, CBT-I addresses the root of the problem, not just the symptoms. Plus, it teaches you skills and techniques you can use for the rest of your life even if your treatment only lasts a few weeks.
If CBT-I sounds like a program that could benefit you, talk to your physician for more information.
Disclaimer: Nolah does not provide medical advice. All resources on the Nolah blog, including this article, are informational only and do not replace professional medical counsel. Talk to your doctor about any health, mental health, or sleep-related issues.
You May Also Like These Articles
Don't Sleep on Exclusive Offers
Sign up for our newsletter, and you'll be the first to know about discounts, deals, and what's new at Nolah.
Ready for Bed?
